Health Plans Partner with Equality Health
Better Health Outcomes – For Those Who Need It Most
With a unique focus on diverse and historically underserved communities, Equality Health partners with providers and health plans to accelerate value-based care so everyone can concentrate on what matters most: the people we all serve.

Providers
Health Plans
Members
Who Is Equality Health?
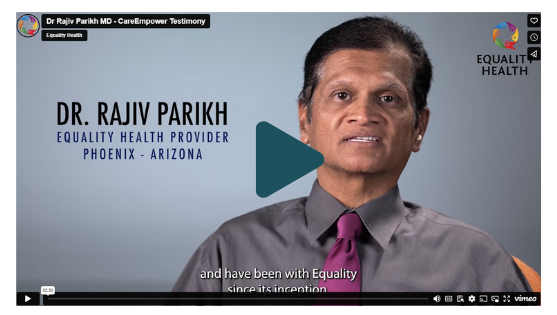
Proudly established in Medicaid, Equality Health is a dynamic value-based care platform dedicated to transforming the current state of healthcare by aligning, engaging, and empowering providers and health plans to focus their work on the individuals and communities that need it the most.
We help ensure that our members and patients receive the highest quality of care and service – no matter their situation, status, or circumstance. We fuse technology, coaching, clinical expertise, financial support, and a deep understanding of value-based payment models to engage plans, providers, patients, and communities in improving whole person care.

25
700K+
Members Supported
3.2K+
Primary Care Providers Participate in the Equality Health Network
5
States Present and Growing